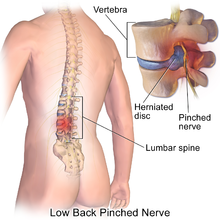
Most authors favour degeneration of the intervertebral disc as the major cause of spinal disc herniation and cite trauma as a low cause. Disc degeneration occurs both with degenerative disc disease and aging. With degeneration, the contents of the disc, the nucleus pulposus and anulus fibrosus, are exposed to altered loads. Specifically, the nucleus becomes fibrous and stiff and less able to bear load. The load is transferred to the anulus, which, if it fails to bear the increased load, can lead to the development of fissures. If the fissures reach the periphery of the anulus, the nuclear material can pass through as a disc herniation.
Disc herniations can result from general wear and tear, such as constant sitting or squatting, driving, or a sedentary lifestyle. However, herniations can also result from the lifting of heavy loads.[citation needed] Professional athletes, especially those playing contact sports such as American football, are prone to disc herniations as well. Within athletic contexts, herniation is often the result of sudden blunt impacts against, or abrupt bending or torsional movements of, the lower back. When the spine is straight, such as in standing or lying down, internal pressure is equalized on all parts of the discs. While sitting or bending to lift, internal pressure on a disc can move from 17 psi (lying down) to over 300 psi (lifting with a rounded back). Herniation of the contents of the disc into the spinal canal often occurs when the anterior side (stomach side) of the disc is compressed while sitting or bending forward, and the contents (nucleus pulposus) get pressed against the tightly stretched and thinned membrane (anulus fibrosus) on the posterior side (back side) of the disc. The combination of membrane thinning from stretching and increased internal pressure (200 to 300 psi) results in the rupture of the confining membrane. The jelly-like contents of the disc then move into the spinal canal, pressing against the spinal nerves, which may produce intense and potentially disabling pain and other symptoms.
Several genes are also associated with intervertebral disc degeneration. Probable candidate genes like type I collagen (sp1 site), type IX collagen, vitamin D receptor, aggrecan, asporin, MMP3, interleukin-1, and interleukin-6 polymorphisms have been implicated in disc degeneration. Mutation in genes coding for proteins involved in the regulation of the extracellular matrix, such as MMP2 and THBS2, has been demonstrated to contribute to lumbar disc herniation.